How childhood trauma causes ‘brain damage’ and how mental health Education develops resilience
Written by Martha Cottam (BSc, MSc Translational Neuroscience)
Why does trauma affect the brain more in early childhood compared to adulthood?
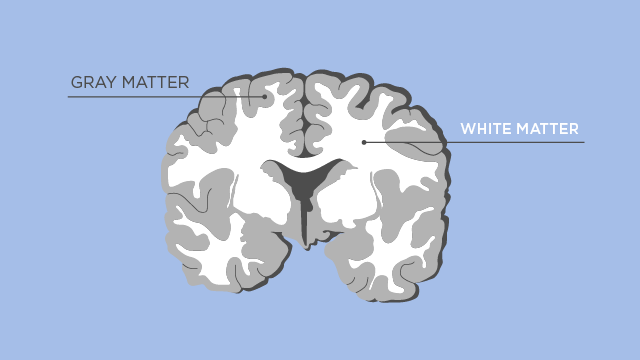
In early life, when an infant begins to explore their social world and acquire knowledge about themselves and others, the brain undergoes dramatic changes. These neural changes are known as ‘plasticity’, the processes the brain undertakes to change and shape itself depending upon our own unique experiences. Through plasticity, new brain cells develop (known as grey matter) and we begin to establish neural connections or pathways which become insulated (or myelinated) to help the brain processes information more rapidly (this is known as white matter). Although plasticity continues throughout our entire lifetime, early childhood is thought to be crucial when mapping out the rest of our brain development as 80-90% of the adult brain volume is formed by the age of 2. Key brain regions responsible for memory, learning, emotion regulation and higher order thinking such as decision making, are all developed in this window of time. These early years are known as a ‘sensitive period’ because the brain is highly responsive to stress. This means that negative adverse experiences can have a detrimental effect on the formation of healthy brain regions and pathways.
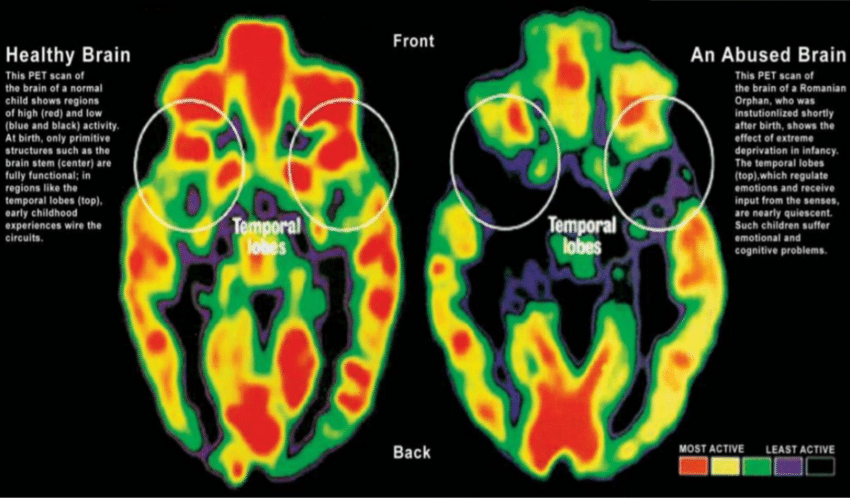
Indeed, over the last decade neuroscience research has illustrated how childhood maltreatment can slow the
development of new brain cells ‘or neurons’ and inhibit the formation of connections between neurons. Additionally, increased early life stress is thought to damage the structural integrity of certain brain areas and alter the wiring of neural circuitry, changing the way neurons communicate with one another. Brain imaging technology such as MRI scanners have allowed scientists to see the effects of childhood abuse on the brain. Neuroscience research has shown that experience of domestic violence or verbal abuse in childhood has a profound effect on the brain, reducing grey matter volume in brain regions responsible for processing this information.
But what does this mean for the individual?
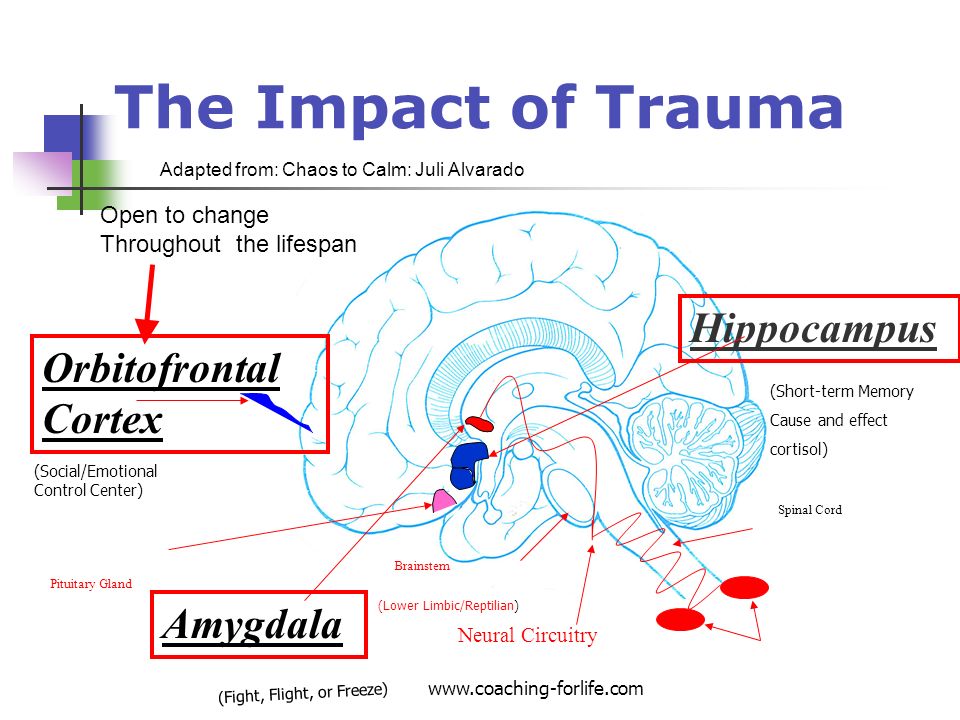
Further neuroscience research has found early life stress can alter brain pathways closely involved in emotion, memory and learning. This may have long lasting impacts on school performance, job outcomes and later life relationships. In one experiment, a group of researchers showed participants a series of pictures showing faces displaying emotions such as joy, sadness, anger and fear. The researchers studied the brain’s response to these pictures in an MRI scanner. The individuals who had suffered early childhood trauma were found to have increased brain activity in the ‘amygdala’, also known as the fear detection centre in the brain. The amygdala became more active when shown sad or fearful faces, compared to those displaying positive emotions. Secondly, the researchers found the brains of abused children responded quicker to negative imagery rather than the positive emotion faces. Taken together, this may suggest the brain is hyper-sensitive to detecting threats or negative stimuli in the environment. Although this would enable the individual to respond much more rapidly with the correct behavioural response, this is ‘built-in-survival-response’ is likely to be a product of our early evolutionary ancestors. This may have negative consequences today as we no longer live in a prehistoric era where threats of wild animals would challenge our day-to-day survival. Therefore, in everyday situations the brains of the individuals who suffered early trauma may be wired in this way to over-identify features of the environment and perceive them as threats. This may lead the individual to continually focus on negative and potentially harmful events or situations which may eventually lead to mental health problems such as depression or anxiety.
But why don’t all children that suffer trauma or abuse develop mental health problems?
A healthy brain architecture would support the ability to be flexible and change with shifting environmental demands, and therefore not be permanently affected by negative events. This is also known as resilience or the ability to ‘bounce back’ from negative experiences.
However, if the brain is under constant stress, the body continues to release stress hormones and neurochemicals that can result in changes to the brain (this is known as allostatic-load). If the individual’s environment is continually negative i.e they are not in a caring supported network and the stress continues, the brain may be unable to return to the healthy ‘set-point’ this is known as ‘allostatic-overload’. Depression, anxiety or Posttraumatic Stress Disorder (PTSD) is characteristic of a brain which is not resilient. This is due a lack of plasticity, leading to fixed brain pathways, low cognitive flexibility and is conceptualized by a constant loop of negative thoughts.
One neuroscience study looked at the structure of the corpus callosum in an MRI scanner (the corpus callosum refers to the middle part of the brain connecting the right and left side). The researchers asked participants if they had suffered early life stress or trauma and recorded their medical history of psychological problems. They found that the brains of individuals who reported adverse childhood stress had a smaller corpus callosum compared to those individuals who had not experienced childhood trauma. This may suggest that early trauma can cause a type of brain damage leaving these individuals susceptible to developing mental health problems. In a second experiment the researchers also gave a questionnaire to the participants to identify personality traits of ‘resilience’. When the experiment was repeated in the brain scanner the research group found that children who experienced early trauma but had high resilience scores did not have smaller corpus callosums. Rather, their brain scan showed their corpus callosum looked more like the brain of the ‘healthy’ participants who had not experienced any early life stress. Additionally, these children did not report any mental health problems such as depression or anxiety.
How can we all re-wire our brain to become resilient?
Intervention therapies aim to increase resilience and reduce the impact of negative mental health problems by stimulating plasticity. Therapies aim to re-wire the brain and reduce structural damage to ensure efficient emotional processing in the brain. Psychological research has shown emotional intelligence training can increase resilience and help people deal with negative life events more effectively. Emotional intelligence is critical for positive mental health as it deals with understanding emotions and how to deal effectively with every-day situations. Improving our emotional intelligence has also been found to improve memory, IQ, school performance, job satisfaction and relationship success.
Another training technique for emotional intelligence is mindfulness meditation, this practices skills of attention and awareness on the individual’s present situation. Mindfulness Meditation has been shown to reduce anxiety and depression by 65% after 8-weeks in individuals wo suffered early-life trauma. The science behind how this works is by helping the brain to re-structure and re-wire the unhealthy brain networks that resulted from the childhood stress. This helps two key brain regions to work together; these are the limbic brain, which deal with emotions and the neocortex or higher functioning brain areas dealing with behavioural inhibition and decision-making. This stops emotional hijacking happening where the emotional brain takes over the thinking brain to cause less rational decision-making. Brain imaging studies have shown practicing mindfulness meditation increases the grey matter in the frontal part of the brain, which is responsible for executive decision making, emotion regulation and working memory. This is critical as these frontal regions of the brain shrink in patients with depression. Other parts of the brain such as the amygdala, the ‘flight or flight’’centre of the brain decreased in size following mindfulness meditation, and as a result the individuals reported decrease in stress levels. Therefore, just by changing the way we think by focusing on the present, we can physically alter the structure of our brain and change how our brain cells communicate with one another. This is through plasticity, as we are gifted with the ability to change our brain throughout the whole of our lifetime simply by changing our thoughts and behaviour. This shows despite any possible negative and stressful life experiences we go through there is potentially always a way of reshaping and restructuring our brains to overcome whatever challenges we may face.
Yours Sincerely,
The Motus Movement.